



Published on Mar 04, 2023
Ayushman Card or Pradhan Mantri Jan Arogya Yojana (PMJAY) will provide financial protection (Swasthya Suraksha) to 10.74 crore poor, deprived rural families and identified occupational categories of urban workers’ families as per the latest Socio-Economic Caste Census (SECC) data (approx. 50 crore beneficiaries). It will have offer a benefit cover of Rs. 500,000 per family per year (on a family floater basis).
PM-JAY will cover medical and hospitalization expenses for almost all secondary care and most of tertiary care procedures. PM-JAY has defined 1,350 medical packages covering surgery, medical and day care treatments including medicines, diagnostics and transport.
Under the ambit of Ayushman Bharat, a Pradhan Mantri Jan Arogya Yojana (PM-JAY) to reduce the financial burden on poor and vulnerable groups arising out of catastrophic hospital episodes and ensure their access to quality health services was conceived. PM-JAY seeks to accelerate India’s progress towards achievement of Universal Health Coverage (UHC) and Sustainable Development Goal - 3.
Telangana has not joined the Pradhan Mantri Jan Arogya Yojana PMJAY Ayushman Bharat, launched by Prime Minister Narendra Modi in Jharkhand Sunday as of now and would continue to implement its health scheme, official sources said Hyderabad: Telangana has not joined the Pradhan Mantri Jan Arogya Yojana PMJAY- Ayushman Bharat, launched by Prime Minister Narendra Modi in Jharkhand Sunday 'as of now' and would continue to implement its health scheme, official sources said. One of the reasons for not joining it, for the time being, was because the state's Aarogyasri scheme covers nearly 80 lakh families, official sources said. "We already have the Aarogyasri scheme. As of now Telangana is not participating in the (central government's) scheme," they told PTI.
Hyderabad: Telangana has not joined the Pradhan Mantri Jan Arogya Yojana PMJAY- Ayushman Bharat, launched by Prime Minister Narendra Modi in Jharkhand Sunday 'as of now' and would continue to implement its health scheme, official sources said. One of the reasons for not joining it, for the time being, was because the state's Aarogyasri scheme covers nearly 80 lakh families, official sources said. "We already have the Aarogyasri scheme. As of now Telangana is not participating in the (central government's) scheme," they told PTI.
Aarogyasri (Rajiv Aarogyasri) was a flagship healthcare program of the Government of Andhra Pradesh before the AP Re-organisation in 2014. After split of state in to Telangana and Andhra Pradesh, Aarogyasri became flagship healthcare scheme of Govt of Telangana and is administered by Aarogyasri Health Care Trust. The new Government of Andhra Pradesh after the state split renamed the scheme in 2014 to Dr NTR Vaidya Seva and is administered by Dr NTR Vaidya Seva Trust. It covers those below the poverty line. The government issues an Aarogyasri card and the beneficiary can use it at government and private hospitals to obtain services free of cost.
Aarogyasri Scheme is the flagship scheme of all health initiatives of the State Government with a mission to provide quality healthcare for the poor. The aim of the Government is to achieve "Health for All". In order to facilitate the effective implementation of the scheme, the State Government set up the Aarogyasri Health Care Trust under the chairmanship of the Chief Minister. The trust is administered by a Chief Executive Officer, an IAS Officer. The trust runs the scheme, in consultation with specialists in the field of healthcare.
The beneficiaries of the scheme are the members of Below Poverty Line (BPL) families as enumerated and photographed in White Ration Card linked with Aadhaar card and available in Civil Supplies Department database. Financial coverage (Height of Universal Health coverage) The scheme shall provide coverage for the services to the beneficiaries up to Rs.2.50 lakh per family per annum on floater basis. There shall be no co-payment under this scheme. Benefit Coverage (Depth of Universal Health coverage)The arogya sri scheme money is eligible to take in both government and private hospitals
The beneficiaries of the scheme, the members of Below Poverty Line (BPL) families, as enumerated and photographed in BPL Ration Card and available in Civil Supplies Department database.
The benefit to the family is on a floater basis i.e. the total reimbursement of Rs.1.50 lakhs can be availed individually or collectively by members of the family. An additional sum of Rs 50,000 is provided as a buffer to take care of expenses if it exceeds the original sum i.e. Rs 1.50 lakhs per family. Excepting cost for cochlear implant surgery with auditory-verbal therapy is reimbursed by the trust up to a maximum of Rs.6.50 lakhs per case.
All transactions are cashless for covered procedures. A BPL beneficiary can go to any hospital either public or private and come out without making any payment to the hospital for the procedures covered under the scheme. The same is the case for diagnostics, if eventually the patient does not end up in undergoing the surgery or therapy.
Hospitals are mandated to conduct free health camp, thereby taking advanced evaluation at the doorstep of patient
1. Households living in only one room with kucha walls and kucha roof.
2. Households with no adult member between age 16 to 59
3. Female headed households with no adult male member between age 16 to 59
4. Households having at least one disabled member and no able-bodied adult member
5. SC/ST households
6. Landless households deriving major part of their income from manual casual labour
7. Households without shelter
8. Destitute/ living on alms
9. Manual scavenger families
10. Primitive tribal groups
11. Legally released bonded labour
• Beggars;
• Rag-pickers;
• Domestic workers;
• Street vendors/cobblers/hawkers/other service providers working on the streets;
• Construction workers/ plumbers/ masons/ labor/ painters/ welders/ security guards/coolies and other head-load workers;
• Sweepers/ sanitation workers/ malis;
• Home-based workers/ artisans/handicrafts workers/ tailors;
• Transport workers/ drivers/ conductors/helpers to drivers and conductors/cart pullers/ rickshaw pullers;
• Shop workers/ assistants/ peons in small establishments/ helpers/ delivery assistants / attendants/ waiters;
• Electricians/ mechanics/ assemblers/repair workers;
• Washer-men/ chowkidars;
• Other work/non-work ;
• Non-work (pension/ rent/ interest, etc.) .
Services under the scheme can be availed at all public hospitals and empaneled private health care facilities. Also, the basic empanelment criteria allows empanelment of a hospital with a minimum of 10 beds, with the flexibility providprovided to states to further relax this if required. Empanelment of the hospitals under AB-NHPM will be conducted through an online portal by the state government. Information about empaneled hospitals will be made available through different means such as government websites and mobile apps. Beneficiaries can also call the helpline number at 14555.
To control costs, the payments for treatment will be done on package rate (to be defined by the Government in advance) basis. However, hospitals with NABH/NQAS accreditation can be incentivised for higher package rates subject to procedure and costing guidelines.
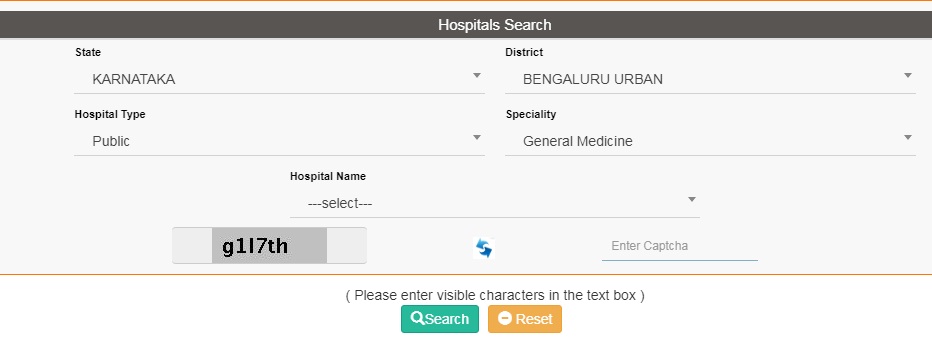
For the list of Hospitals, Kindly click the below link and Type as follows.
Visit https://hospitals.pmjay.gov.in/Search/empnlWorkFlow.htm?actionFlag=ViewRegisteredHosptlsNew
1. Select State
2. Select District
3. Select Hospital Type - Public, Private (Not for Profit) or Private(For Profit)
4. Select Speciality - General Medicine, Paediatric medical management, Neo-natal, Paediatric cancer, Emergency Room Packages, etc ......
5. Enter Captcha as shown
6. Lastly Enter Search.
Now you will get the list of Hospitals which is covered by Ayushman Bharat.

1. Government provides health insurance cover of up to Rs. 5,00,000 per family per year.
2. More than 10.74 crore poor and vulnerable families (approximately 50 crore beneficiaries) covered across the country.
3. All families listed in the SECC database as per defined criteria will be covered. No cap on family size and age of members.
4. Priority to girl child, women and and senior citizens.
5. Free treatment available at all public and empaneled private hospitals in times of need.
6. Covers secondary and tertiary care hospitalization.
7. 1,350 medical packages covering surgery, medical and day care treatments, cost of medicines and diagnostics.
8. All pre-existing diseases covered. Hospitals cannot deny treatment.
9. Cashless and paperless access to quality health care services.
10. Hospitals will not be allowed to charge any additional money from beneficiaries for the treatment.
11. Eligible beneificiares can avail services across India, offering benefit of national portability. Can reach out for information, assistance, complaints and grievances to a 24X7 helpline number - 14555
1. Go to NHA portal and Log in to mera.pmjay.gov.in
2. Enter your mobile number and captcha code.
3. A one-time password will be sent to your mobile number.
4. After entering the OTP, you will be taken to this screen.
5. Select the state: Fill all the fields like name, mobile number, ration card number, or Rashtriya Swasthya Bima Yojna URN number.
6. If your name is there in the list, it will show up on the right-hand side of the page.
7. Click on 'Family Members' tab to find the beneficiary details
• Respective special category certificates
• Age proof documents
• Family structure
• Identification details
• Contact information
• Scanned copy of Aadhar
• Income certificate
• Caste certificate