



Published on Oct 30, 2018
Press Information Bureau
Government of India
Ministry of Finance
01-February-2018 13:31 IST
Ayushman Bharat for a new India -2022, announced
1. Two major initiatives in health sector announced
2. Rs. 1200 Crore allocated for 1.5 Lakh health and wellness Centres
3. National health protection Scheme to provide Hospitalisation cover to over 10 Crore poor and vulnerable families
The Government today announced two major initiatives in health sector , as part of Ayushman Bharat programme. The Union Minister for Finance and Corporate Affairs, Shri Arun Jaitely while presenting the General Budget 2018-19 in Parliament here today said that this was aimed at making path breaking interventions to address health holistically, in primary, secondary and tertiary care systems, covering both prevention and health promotion.
The initiatives are as follows:-
The National Health Policy, 2017 has envisioned Health and Wellness Centres as the foundation of India’s health system. Under this 1.5 lakh centres will bring health care system closer to the homes of people. These centres will provide comprehensive health care, including for non-communicable diseases and maternal and child health services. These centres will also provide free essential drugs and diagnostic services. The Budget has allocated Rs.1200 crore for this flagship programme. Contribution of private sector through CSR and philanthropic institutions in adopting these centres is also envisaged.
The second flagship programme under Ayushman Bharat is National Health Protection Scheme, which will cover over 10 crore poor and vulnerable families (approximately 50 crore beneficiaries) providing coverage upto 5 lakh rupees per family per year for secondary and tertiary care hospitalization. This will be the world’s largest government funded health care programme. Adequate funds will be provided for smooth implementation of this programme.
The Finance Minister further said, that these two health sector initiatives under Ayushman Bharat Programme will build a New India 2022 and ensure enhanced productivity, well being and avert wage loss and impoverishment. These Schemes will also generate lakhs of jobs, particularly for women.
The Finance Minister said, that in order to further enhance accessibility of quality medical education and health care, 24 new Government Medical Colleges and Hospitals will be set up, by up-grading existing district hospitals in the country. This would ensure that there is at least 1 Medical College for every 3 Parliamentary Constituencies and at least 1 Government Medical College in each State of the country.
Ayushman Bharat or Pradhan Mantri Jan Arogya Yojana is National Health Protection Scheme, which will cover over 10 crore poor and vulnerable families (approximately 50 crore beneficiaries) providing coverage upto 5 lakh rupees per family per year for secondary and tertiary care hospitalization. Ayushman Bharat - National Health Protection Mission will subsume the on-going centrally sponsored schemes - Rashtriya Swasthya Bima Yojana (RSBY) and the Senior Citizen Health Insurance Scheme (SCHIS).
Ayushman Bharat (AB) is an attempt to move from sectoral and segmented approach of health service delivery to a comprehensive need-based health care service. Ayushman Bharat aims to undertake path breaking interventions to holistically address health (covering prevention, promotion and ambulatory care), at primary, secondary and tertiary level. Ayushman Bharat adopts a continuum of care approach, comprising of two inter-related components.
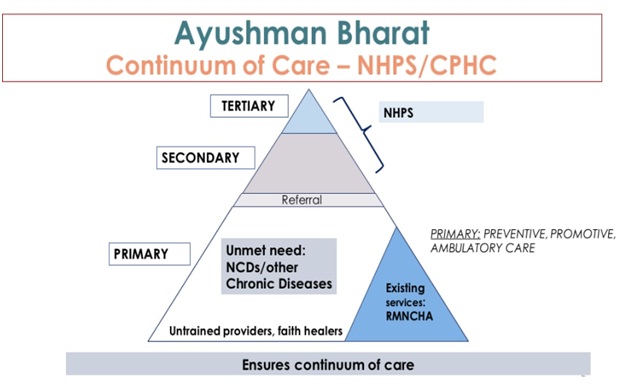
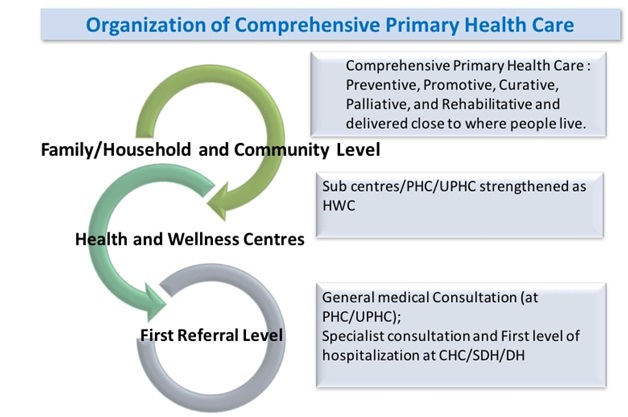
The first component, pertains to creation of 1,50,000 Health and Wellness Centres which will bring health care closer to the homes of the people. These centres will provide Comprehensive Primary Health Care (CPHC), covering both maternal and child health services and non-communicable diseases, including free essential drugs and diagnostic services. The first Health and Wellness Centre was launched by the Hon’ble Prime Minister at Jangla, Bijapur, Chhatisgarh on 14 April 2018. The second component is the Pradhan Mantri Jan Arogya Yojana (PM-JAY) which provides health protection cover to poor and vulnerable families. The Health and Wellness Centres will play a critical role in creating awareness about PM-JAY, screening for non-communicable diseases, follow-up of hospitalisation cases among others.
• Ayushman Bharat - National Health Protection Mission will have a defined benefit cover of Rs. 5 lakh per family per year.
• Benefits of the scheme are portable across the country and a beneficiary covered under the scheme will be allowed to take cashless benefits from any public/private empanelled hospitals across the country.
• Ayushman Bharat - National Health Protection Mission will be an entitlement based scheme with entitlement decided on the basis of deprivation criteria in the SECC database.
• The beneficiaries can avail benefits in both public and empanelled private facilities.
• To control costs, the payments for treatment will be done on package rate (to be defined by the Government in advance) basis.
• One of the core principles of Ayushman Bharat - National Health Protection Mission is to co-operative federalism and flexibility to states.
• For giving policy directions and fostering coordination between Centre and States, it is proposed to set up Ayushman Bharat National Health Protection Mission Council (AB-NHPMC) at apex level Chaired by Union Health and Family Welfare Minister.
• States would need to have State Health Agency (SHA) to implement the scheme.
• To ensure that the funds reach SHA on time, the transfer of funds from Central Government through Ayushman Bharat - National Health Protection Mission to State Health Agencies may be done through an escrow account directly.
• In partnership with NITI Aayog, a robust, modular, scalable and interoperable IT platform will be made operational which will entail a paperless, cashless transaction.
1. Households living in only one room with kucha walls and kucha roof.
2. Households with no adult member between age 16 to 59
3. Female headed households with no adult male member between age 16 to 59
4. Households having at least one disabled member and no able-bodied adult member
5. SC/ST households
6. Landless households deriving major part of their income from manual casual labour
7. Households without shelter
8. Destitute/ living on alms
9. Manual scavenger families
10. Primitive tribal groups
11. Legally released bonded labour
• Beggars;
• Rag-pickers;
• Domestic workers;
• Street vendors/cobblers/hawkers/other service providers working on the streets;
• Construction workers/ plumbers/ masons/ labor/ painters/ welders/ security guards/coolies and other head-load workers;
• Sweepers/ sanitation workers/ malis;
• Home-based workers/ artisans/handicrafts workers/ tailors;
• Transport workers/ drivers/ conductors/helpers to drivers and conductors/cart pullers/ rickshaw pullers;
• Shop workers/ assistants/ peons in small establishments/ helpers/ delivery assistants / attendants/ waiters;
• Electricians/ mechanics/ assemblers/repair workers;
• Washer-men/ chowkidars;
• Other work/non-work ;
• Non-work (pension/ rent/ interest, etc.) .
The beneficiaries will not be required to pay any charges and premium for the hospitalisation expenses. The benefit also include pre- and post-hospitalisation expenses.
Each empanelled hospital will have an 'Ayushman Mitra' to assist patients and will coordinate with beneficiaries and the hospital. They will run a help desk, check documents to verify the eligibility, and enrolment to the scheme.
Also, all the beneficiaries will be given letters having QR codes which will be scanned and a demographic authentication will be conducted for identification and to verify his or her eligibility to avail the benefits of the scheme.
Benefits of the scheme are portable across the country and a beneficiary covered under the scheme will be allowed to take cashless benefits from any public/private empanelled hospitals across the country.
There is no enrolment process in AB-NHPM as it is an entitlement-based mission. Families who are identified by the government on the basis of deprivation and occupational criteria using the SECC database, both in rural and urban areas, are entitled for AB-NHPM. Currently the database is based on census for the year 2011.
A list of eligible families has been shared with the respective state governments as well as state level departments like the ANMs, BMO, and BDOs of relevant areas. A dedicated AB-NHPM family identification number will be allotted to eligible families. Only families whose name is on the list are entitled for the benefits of AB-NHPM.
Additionally, families with an active RSBY cards as of 28 February 2018 will covered. No additional new families can be added under AB-NHPM. However, names of additional family members can be added for those families whose names are already on the on the SECC list.
The official website of AB-NHPM is www.abnhpm.gov.in . One may visit the site to view and download the beneficiary eligibility and empanelled hospitals list as and when it gets updated.
Services under the scheme can be availed at all public hospitals and empaneled private health care facilities. Also, the basic empanelment criteria allows empanelment of a hospital with a minimum of 10 beds, with the flexibility providprovided to states to further relax this if required. Empanelment of the hospitals under AB-NHPM will be conducted through an online portal by the state government. Information about empaneled hospitals will be made available through different means such as government websites and mobile apps. Beneficiaries can also call the helpline number at 14555.
To control costs, the payments for treatment will be done on package rate (to be defined by the Government in advance) basis. However, hospitals with NABH/NQAS accreditation can be incentivised for higher package rates subject to procedure and costing guidelines.
1. Government provides health insurance cover of up to Rs. 5,00,000 per family per year.
2. More than 10.74 crore poor and vulnerable families (approximately 50 crore beneficiaries) covered across the country.
3. All families listed in the SECC database as per defined criteria will be covered. No cap on family size and age of members.
4. Priority to girl child, women and and senior citizens.
5. Free treatment available at all public and empaneled private hospitals in times of need.
6. Covers secondary and tertiary care hospitalization.
7. 1,350 medical packages covering surgery, medical and day care treatments, cost of medicines and diagnostics.
8. All pre-existing diseases covered. Hospitals cannot deny treatment.
9. Cashless and paperless access to quality health care services.
10. Hospitals will not be allowed to charge any additional money from beneficiaries for the treatment.
11. Eligible beneificiares can avail services across India, offering benefit of national portability. Can reach out for information, assistance, complaints and grievances to a 24X7 helpline number - 14555
• Help India progressively achieve Universal Health Coverage (UHC) and Sustainable Development Goals (SDG).
• Ensure improved access and affordability, of quality secondary and tertiary care services through a combination of public hospitals and well measured strategic purchasing of services in health care deficit areas, from private care providers, especially the not-for profit providers.
• Significantly reduce out of pocket expenditure for hospitalization. Mitigate financial risk arising out of catastrophic health episodes and consequent impoverishment for poor and vulnerable families.
• Acting as a steward, align the growth of private sector with public health goals.
• Enhanced used to of evidence based health care and cost control for improved health outcomes.
• Strengthen public health care systems through infusion of insurance revenues.
• Enable creation of new health infrastructure in rural, remote and under-served areas.
• Increase health expenditure by Government as a percentage of GDP.
• Enhanced patient satisfaction. • Improved health outcomes.
• Improvement in population-level productivity and efficiency
• Improved quality of life for the population
1. Go to NHA portal and Log in to mera.pmjay.gov.in
2. Enter your mobile number and captcha code.
3. A one-time password will be sent to your mobile number.
4. After entering the OTP, you will be taken to this screen.
5. Select the state: Fill all the fields like name, mobile number, ration card number, or Rashtriya Swasthya Bima Yojna URN number.
6. If your name is there in the list, it will show up on the right-hand side of the page.
7. Click on 'Family Members' tab to find the beneficiary details
• Respective special category certificates
• Age proof documents
• Family structure
• Identification details
• Contact information
• Scanned copy of Aadhar
• Income certificate
• Caste certificate
As many as 194 government and private hospitals in Haryana have been empanelled for the Centre's Ayushman Bharat Scheme, Health Minister Anil Vij said on Wednesday.
Vij said that Haryana is the first state to start this health insurance facility on a pilot basis from August 15. It will be implemented in one government hospital each in 22 districts of the state.
On getting private hospitals on board, Bhushan said NHA has made quite a progress.
"So far, nearly 9,000 private hospitals have got empanelled in the scheme, and another 3,000 applications are pending with the agency. We will clear them in the days to come," Bhushan said.
Bhushan added that large hospital chains like Medanta have joined the scheme, while Apollo Hospitals and Narayana Health expressed interest and will soon be part of the scheme.
Bhushan said with Tamil Nadu and Karnataka signing MoUs, "we expect Apollo and Narayana Health to be part of the scheme, as both the hospital chains are part of the respective states' health assurance schemes".
Prime Minister Narendra Modi will inaugurate the nationwide scheme on September 23 from Ranchi, wherein 10 crore poor and vulnerable families across the country, including 15.50 lakh families in Haryana, will be provided cashless coverage of up to Rs 5 lakh per family per year for secondary and tertiary care hospitalisation.
It will be the world's largest government-funded healthcare programme.
The Health Minister said that the state's people have started getting benefits under this scheme. So far, 35 persons have claimed aid under this scheme and 18 of them have already received the money, he claimed.
Similarly, 126 persons have been admitted to hospitals and 4,556 included in 'Golden Record' after their examination.
Vij also said that 'Ayurveda Mitras' are being deputed in state hospitals for assisting patients.
Twenty-four of the 36 states and union territories have one or the other scheme covering a stipulated population for cashless insurance services. Most of these schemes will be subsumed under Ayushman Bharat. Also, hospitals already empanelled under the Rashtriya Swasthya Bima Yojana (RSBY) need not register online again.
Dr Indu Bhushan, CEO, National Health Agency and Ayushman Bharat said, “I call upon each one of you to partner with the mission through the empanelment process initiated today to enhance accessibility for the people who need it most. I also request all the states/ UT governments to help us garner the support of hospitals and healthcare providers in this path-breaking mission.”
“We are also making every effort to ensure that the empanelment process is conducted in a transparent, time-bound and non-partisan manner based on specific criteria, eligibility and guidelines,” Dr Dinesh Arora, Deputy CEO of Ayushman Bharat said.
Besides, 22 District Nodal Officers and 22 District IT Managers have also been engaged for the scheme's implementation.
AB-NHPM will be rolled out across all States/UTs in all districts with an objective to cover all the targeted beneficiaries.
RSBY was launched in the year 2008 by the Ministry of Labour and Employment and provides cashless health insurance scheme with benefit coverage of Rs. 30.000/- per annum on a family floater basis [for 5 members], for Below Poverty Line (BPL) families, and 11 other defined categories of unorganised workers. To integrate RSBY into the health system and make it a part of the comprehensive health care vision of Government of India, RSBY was transferred to the Ministry of Health and Family Welfare (MoHFW) w.e.f 01.04.2015. During 2016-2017, 3.63 crore families were covered under RSBY in 278 districts of the country and they could avail medical treatment across the network of 8,697 empanelled hospitals. The NHPS comes in the backdrop of the fact that various Central Ministries and State/UT Governments have launched health insurance/ protection schemes for their own defined set of beneficiaries. There is a critical need to converge these schemes, so as to achieve improved efficiency, reach and coverage.