https //tms.pmjay.gov.in/one tms : Transaction Management System (TMS) – Ayushman Bharat
Transactions Management System can be accessed by logging on to the website https://tms.pmjay.gov.in/OneTMS. On the landing page, kindly enter your Username and Password. State selection will happen automatically to CAPF.
The flagship scheme of Hon’ble Prime Minister of India was launched in the State of Goa on 23rd September 2018, along with National launch.
- Your family name could be covered in the PMJAY beneficiary list.
- To check out if you are a beneficiary, you can login here using your mobile number.
- You do not need to enroll anywhere to claim benefits under the scheme.
- To claim benefits under the scheme you can get yourself identified at the nearest empanelled hospital or Community Service Centre (CSC)
Accessing Transactions Management System Portal
Upon empanelment of the hospital, each official will be given a unique username and password based on their role in the Hospital Transactions Management workflow; i.e. Medical Coordinator (MEDCO), Preauth Panel Doctor (PPD), Claims Panel Doctor (CPD), Claims Executive (CEX) and Accounts Officer (ACO). If you have not received username and password to access the system or for any other technical issue, please contact support.pmjay.gov.in through your respective SHA or District Coordinators.
Databricks IPO Date 2021: Databricks IPO Price, News, Plans, Launch
a) Transactions Management System can be accessed by logging on to the website https://tms.pmjay.gov.in/OneTMS
b) On the landing page, kindly enter your Username and Password. State selection will happen automatically to CAPF
c) Enter the captcha visible on the screen. Refresh if you do not see the captcha.
d) Agree to terms, eligibility criteria and data policy by clicking on the checkbox displayed on the screen.
e) Click on Login to proceed.
Also Read : https //beneficiary.nha.gov.in
Objective of the Scheme:
The objective of AB-PMJAY is to reduce catastrophic health expenditure, improve access to quality health care, reduce unmet needs and reduce out of pocket healthcare expenditures of poor and vulnerable families of the Socio-Economic Caste Census (SECC) 2011 database of the State/ UT along with the estimated existing RSBY Beneficiary Families not figuring in the SECC database.
Cowboy Bebop Live Action Release : Cowboy Bebop Netflix Review
Salient features of the scheme:
a. AB-PMJAY is the world’s largest health insurance/ assurance scheme fully financed by the government.
b. It provides a cover of Rs. 5 lakhs per family per year for secondary and tertiary care hospitalization across public and private empanelled hospitals in India.
c. PM-JAY has defined 1,650 medical packages in Goa.
d. Over 10.74 crore poor and vulnerable entitled families (approximately 50 crore beneficiaries) are eligible for these benefits.
e. PM-JAY provides cashless access to health care services for the beneficiary at the point of service, that is, the hospital.
f. There is no restriction on the family size, age or gender.
g. Benefits of the scheme are portable across the country i.e. a beneficiary can visit any empanelled public or private hospital in India to avail cashless treatment.
Core features:
• A cover of Rs. 5 Lakh per family per year
• Over 10 Crore poor and vulnerable families eligible
• States given flexibility to decide on mode of implementation
• Benefits will be portable across the country
• Entitlement based scheme
Overview
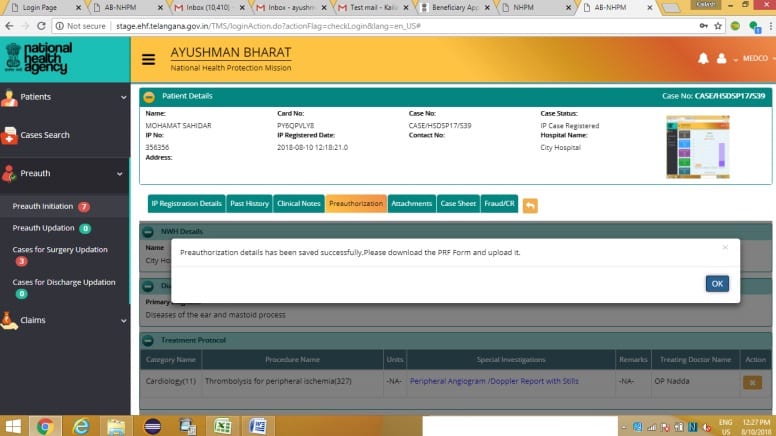
Patient hospitalization>Beneficiary Identification & Registration> Pre- Authorization Request & Approval > Treatment> claim request & Approval > Discharge
• Cover uptoRs. 5Lac/family/ year
• <10.74 crore SECC++ beneficiaries
• Completely cashless & paperless
• 1,350+ medical packages at empanelled hospitals
• Integrated IT systems based Ecosystem
• Privacy & confidentialiality ensured
Service Coverage
Inclusions
• 1350 treatment packages
• Family deductible bucket of INR 5,00,000
• Secondary & Tertiary care IP services including day care procedures
• Pre-existing conditions
• New born care
• Pre- authorization for defined packages
• Provision to cover ‘unspecified surgical conditions’, on pre-authorization p to a limit of INR 1,00,000
Exclusion
• Out- patient care
• Individual diagnostics (for evaluation)
• Drug rehabilitation program
• Cosmetic related
• Fertility related
• Transplants involving organs etc.
What constitutes treatment package?
End to end coverage for entire episode of care
• Medical examination, treatment and consultation
• Pre- hospitalization (3 days)
• Medicine and medical consumables
• Non- intensive and intensive care services
• Diagnostic and laboratory investigation
• Medical implant services (where necessary)
• Accommodation benefits
• Food services
• Complication arising during treatment
• Post- hospitalization (15 days) – at discharge medicines
Claim settlement process
EHCP raises claims> claims management team review claims >claim approved> claims payment on weekly basis- transfer to bank account
Claims rejection > share reasons for rejection
Further inspection > review on fortnightly basis
(within 15 days, inter state within 30 days)
• SHA will approve or reject a claim within 15 calendar days (Turn Around Time) from the date or calm submission
• SHA may collect diagnostic reports from EHCP for adult purpose
• EHCP can appeal to district grievance (DGC) to review the claim, within 30 days of claim rejection