Aetna Extra Benefits Card 2024 Activate Login
Your Aetna D-SNP gives you an Aetna Extra Benefits Card to help you pay for certain everyday expenses. The Extra Benefits Card will be automatically loaded with your Wallet allowance amount(s) each month.
Aetna® Dual Eligible Special Needs Plans, or D-SNPs, give you an Aetna Medicare Extra Benefits Card to help pay for everyday expenses like healthy foods, over-the-counter health products and even rent.
That’s on top of our medical coverage and $0 copay for covered Part D prescriptions at in-network pharmacies. Plus, we offer D-SNPs with dental, vision and hearing benefits.
We make it easy, too. If you’re a new member, we’ll mail you an Extra Benefits Card, a Benefits Mastercard® Prepaid Card, with monthly allowances called “Wallets.”
If you’re a returning member, you can continue to use the Extra Benefits Card you already have — be sure to hold on to it. You’ll receive a letter from NationsBenefits explaining your card changes and new Wallets.
All D-SNP members get Wallets they can use to buy healthy foods like fruits and veggies, meat and seafood, healthy grains like bread and pasta and pantry staples like flour and spices.
You can also buy select over-the-counter, or OTC, health and wellness items, like pain relievers, cold and flu medications and first aid supplies.
The Extra Supports Wallet is our most flexible allowance. It can be used to help pay for healthy foods and OTC items along with several other approved products and services, including:
- Rent or mortgage assistance
- Personal care items
- Utilities
- Transportation
- And pet care items
Wallets vary by plan. Check coverage in your area.
Your Extra Benefits Card will come with information on how and where you can use your card as well as your Wallet amounts.
How to Activate it
To use your card, you’ll need to activate it. You can do that three ways.
1. Phone. Call 1-877-204-1817 (TTY: 711) to speak with a Member Experience Advisor. The number is also on your Extra Benefits Card.
2. QR code. Simply scan the QR code in your Extra Benefits Card welcome materials.
3. Online. Go to Aetna.NationsBenefits.com/Activate
Once your card is activated, your funds are available to spend. You can spend them however you like on any approved products or services.
Not sure if an item is approved for purchase? It’s easy to look up covered items using the NationsBenefits mobile app on your smartphone. The app is available for free on the App Store® and the Google Play™ store.
The Extra Benefits Card can be used at approved retail locations. At checkout, simply swipe your card and select credit when prompted for payment type. No PIN is required.
If your Extra Benefits allowance covers your full purchase, you’re good to go. You’ll need to use a different payment method if any of your items or services aren’t approved, or to pay for the remainder if you’ve used up your allowance. You can check your balance at any time on the NationsBenefits app.
Your Extra Benefits Card helps you put your health first so you can feel your best. To learn more, visit Aetna.NationsBenefits.com
Check your Wellness Credit Balance
1. Go to the Aetna website.
2. Log in with your user ID and password. If you are not a registered user, you will need to sign up by using information on your Aetna member card.
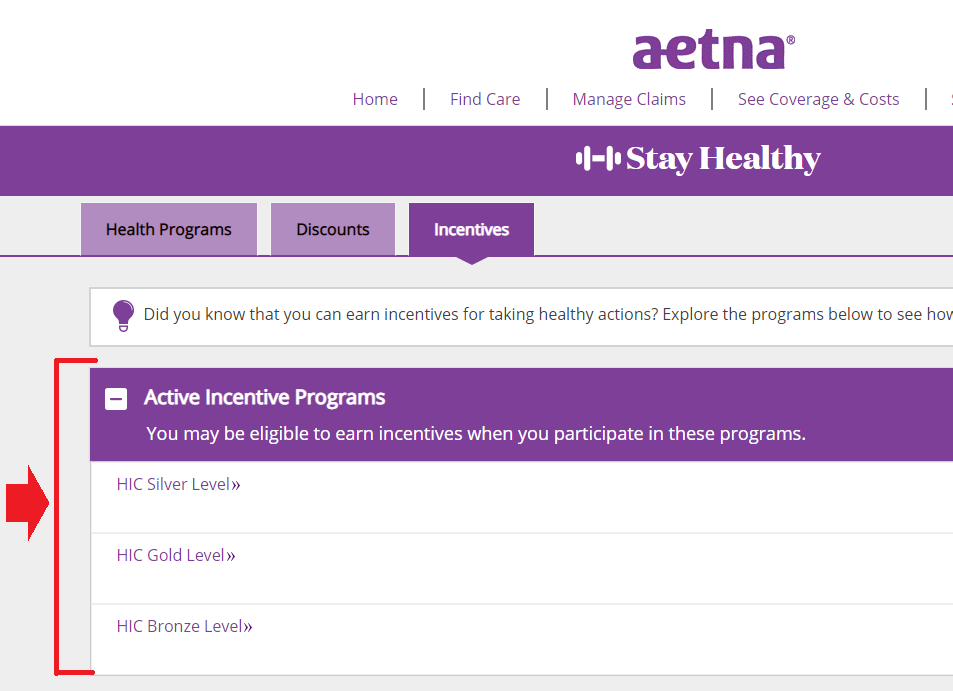
3. Once you are logged in, select Health & Wellness from the menu
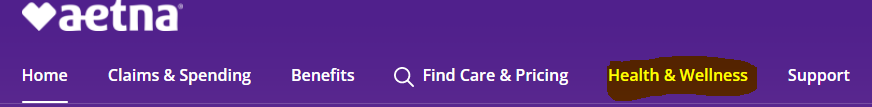
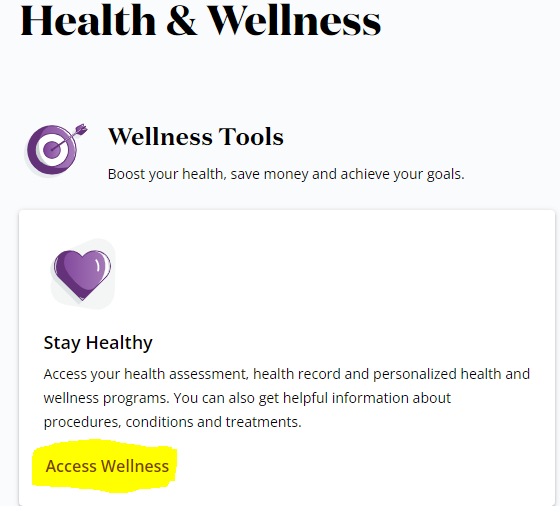
4. Scroll down to Wellness Tools and select Access Wellness
5. Next you will see the Incentive Reward Programs screen. Under Active Incentive Programs, choose your completed Go for the Gold program level for the current year. The Expired Incentive Programs section below will show your incentive rewards earned in previous years.
6. After clicking on your program level, you will then be directed to the program level page showing your wellness credit earned.
Features of the NationsOTC Solution:-
1. CMS-compliant and fully customizable program.
2. 24/7/365 live customer service.
3. Comprehensive product formulary, including healthy foods and connectivity devices.
4. Competitive product pricing
5. Five national distribution centers
6. Nationwide 2-day delivery, at no additional cost
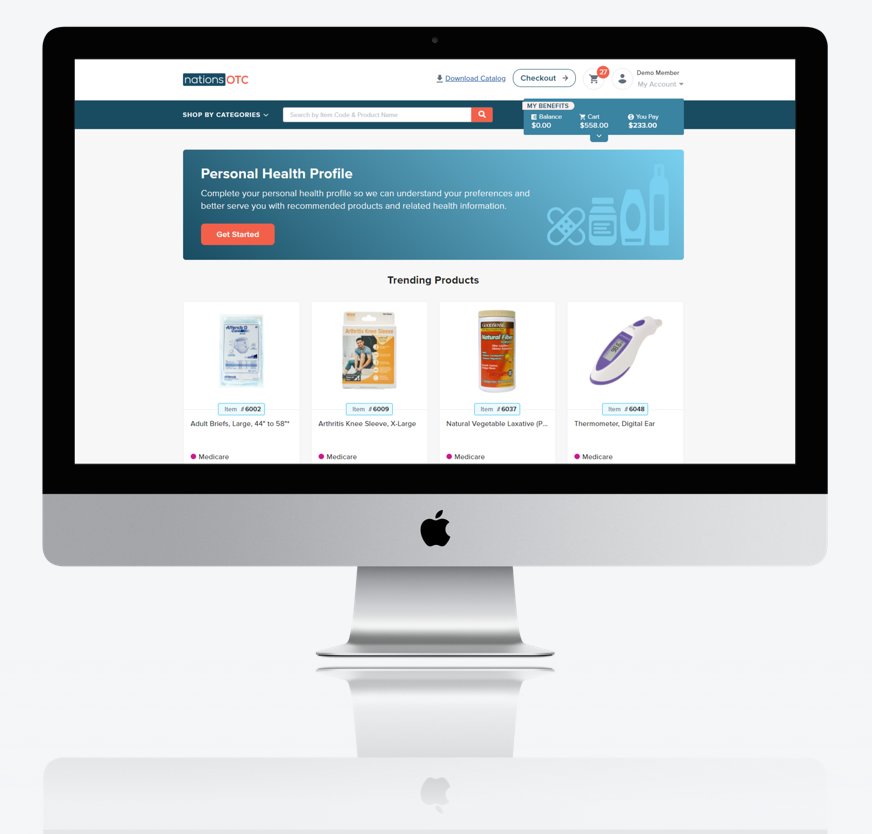
Member Portal
Create additional brand affinity by featuring your logo on the portal, which offers:-
- Robust search options with the ability to filter, sort and search by category, pricing, wallet, and more
- Product recommendations based on individual needs
- Expandable product detail pages complete with 360-degree images
- Benefit tracking to see available dollars to spend on plan-approved products
- Order tracking with carrier details and frequent status updates
Aetna Extra Benefits Card 2023
Open the Member Portal and the page will be redirect you to the member portal for profile registration. After completing registration, you will be prompted to activate your card if you have OTC Card in your hands.
How does the card work?
Starting January 1, we load the card every quarter with $100. Members can use the card to pay for in-network copayments when visiting a primary care physician (PCP) office, a specialist office, and offices that perform certain other types of services.
If your office accepts Mastercard®, the member can swipe the card as a debit card (with or without a PIN) to pay the copayment amount. The member can pay the full amount in this way. Or, if your office allows the use of more than one payment method, the member can opt to pay a portion of the amount with the card and use a different payment method for the rest of the amount.
What if the card doesn’t work or is declined?
- Make sure the member is using the card only for a copayment.
- The card hasn’t been activated. The member can activate their card by calling the number on their activation sticker. That number is 1-877-261-9951 (TTY: 711). The member should call that number to activate the card and then try to pay again.
- The expense might not be considered eligible under the plan. The member should refer to their Explanation of Coverage (EOC) document.
Need help getting started?
If you have any questions, please call us at 877-439-2665(TTY: 711).
Member Experience Advisors are available 24 hours per day, 7 days per week, 365 days per year. Language support services are available free of charge.
FAQs
How do I use my Aetna Healthy Benefits card?
- Always select credit when using the card – a PIN is never needed.
- You can also shop online or by phone.
- Online: Visit Aetna.NationsBenefits.com, log in and shop for approved food products.
- By phone: Call 1‑877‑204‑1817 (TTY: 711) and speak to a representative who can assist you with your order.
What is the Aetna card used for?
The Aetna Extra Benefits Card can help with certain everyday expenses. Aetna® Dual Eligible Special Needs Plans, or D-SNPs, give you an Aetna Medicare Extra Benefits Card to help pay for everyday expenses like healthy foods, over-the-counter health products and even rent.
What is group ID on Aetna insurance card?
Each employer that purchases a health plan for its employees also has a number. This group number identifies the specific benefits associated you your employer’s plan. Healthcare providers use the group number plus your member ID number to file claims for your care.
Where is my subscriber ID on Aetna?
You can find your Member ID on your ID card, Welcome Letter, or any EOB we sent to you.
What does nap mean on my Aetna card?
NAP stands for National Advantage Program. You may get a discount if you use a NAP doctor. However, a discount cannot be guaranteed under the NAP for any particular claim. But… and it’s important: NAP doctors are NOT in-network for your plan.
Is Aetna Better Health of Kansas a Medicaid plan?
Aetna Better Health of Kansas is part of Aetna® and the CVS Health® family, one of our country’s leading health care organizations. We’ve been serving people who use Medicaid services for over 30 years — from kids, adults and seniors to people with disabilities or other serious health issues.
How do I check my balance on my Healthy Food Benefit card?
Quickly and easily check the balance on your card without logging into your account! Simply enter your card number and security code, which may be located on either the front or back of your card.